Did you know? Only 25% of people with heart disease know about the power of activating the vagus nerve, despite mounting evidence showing its profound impact on longevity and heart health. While most focus on diet and exercise, nerve stimulation—particularly of the vagus nerve—could be the missing link to cardiovascular wellness. In this opinion piece, I’ll share the surprising science, personal reflections, and practical steps for harnessing the vagus nerve’s potential to transform your well-being.
A Startling Statistic: The Overlooked Impact of Activating Vagus Nerve
It’s astonishing how vast the gap is between what researchers know and what the public widely practices. Major clinical trials and the Centers for Medicare have reported that interventions activating the vagus nerve produce measurable changes in heart rate and lower systemic inflammation. Yet, activating vagus nerve is still a footnote in most mainstream conversations about heart health, often eclipsed by more familiar lifestyle changes.
The real surprise lies in the data: Individuals who engage in consistent vagus nerve stimulation—even via everyday methods—demonstrate a reduction in resting heart rate and improved heart variability compared to control groups receiving standard therapy. With interventions as simple as deep breathing or brief cold exposure, the heart’s resilience and adaptability strengthen over time. As a society, by overlooking the vagus nerve, we may be missing one of the most accessible and profound levers for unlocking cardiovascular longevity.
The Unconventional Connection Between Vagus Nerve and Longevity
When we explore the relationship between the vagus nerve and long life, the science points to a clear trend: higher vagal tone, often measured by heart rate variability, correlates with better cardiovascular health and even longevity. This nerve acts as a top-down regulator, modulating signals between the brain and vital internal organs. By activating vagus nerve, there’s not just short-term calm but cellular, systemic changes that stand to protect the heart against chronic wear and tear associated with aging. Emerging evidence also links this neurological signaling to a slowed aging process—something highly coveted among heart and wellness researchers.
The field is still young, but studies of markedly improved autonomic resilience suggest those engaging in intentional nerve stimulation may experience more years free of cardiovascular disease. In other words, while medical therapies address symptoms at the end stage, activating the vagus nerve targets the body’s intrinsic self-repair systems. For those seeking to optimize their healthspan, this unconventional but evidence-supported pathway deserves more attention.
How Cardiovascular Health Depends on Activating Vagus Nerve
Your heart is not an island; it operates under guidance, much of which comes from the vagus nerve—the command bridge between brain, heart, and major organs. Activating vagus nerve isn’t merely a stress reducer; it orchestrates a shift into “rest and digest” mode, dropping heart rate and easing the heart’s metabolic workload. This transition is measurable not only in subjective calm but in tangible clinical metrics.
The mechanisms at play go deep. Nerve stimulation modulates both electrical pulses and inflammation, key contributors to quality of life for those with heart or autoimmune conditions. According to a recent international journal study, even non-invasive stimulation (such as slow, deep breathing or gently submerging in cold water) initiates a cascade that improves heart rhythm and circulatory function. Researchers found this highly atypical intervention outperforms many traditional heart therapies—without drugs or surgery. When it comes to true cardiovascular wellness, activating the vagus nerve shifts the odds in your favor.
What You'll Learn About Activating Vagus Nerve
- Key Takeaways on activating vagus nerve: Understand the foundational science and why stimulating this nerve matters for your health.
- Vagus nerve stimulation: Learn about clinical and at-home methods that actually work—and how they compare to standard treatments.
- Nerve stimulation techniques: Discover actionable, evidence-backed techniques—from ice baths to mindfulness—for daily implementation.
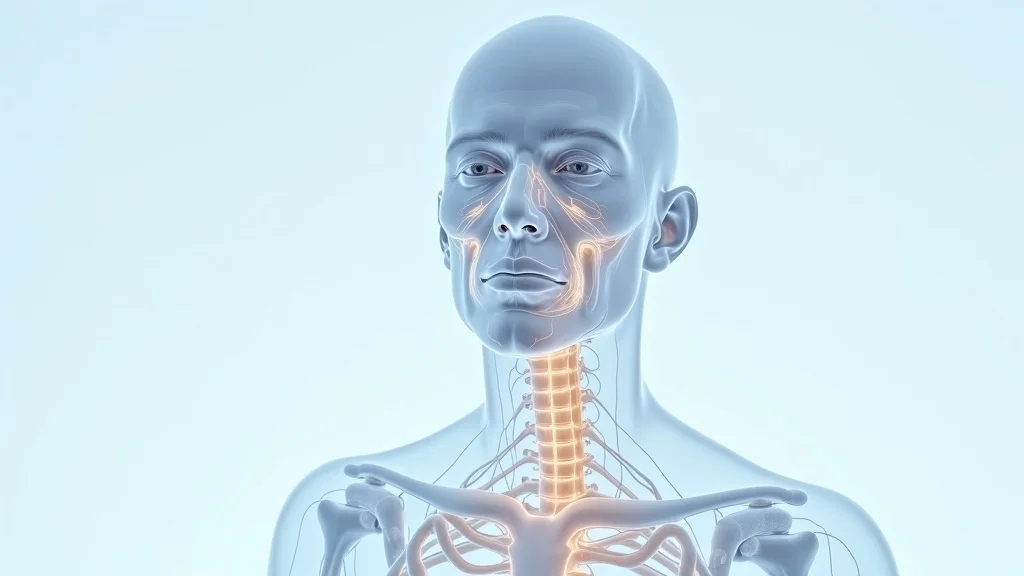
Understanding the Vagus Nerve: Anatomy and Function
Vagus Nerve Basics: What It Is and Why It Matters
The vagus nerve is the body’s largest cranial nerve, running from the brainstem all the way through the neck and torso, branching into virtually every major internal organ. This remarkable nerve acts as a two-way communication road, keeping the brain in constant dialogue with the heart, lungs, gut, and more. It’s not just a scientific curiosity—activating vagus nerve directly affects daily function, regulating everything from heart rate and blood pressure to mood and digestive health.
Why does this matter? Because the health of this “wandering” nerve is now understood to be a cornerstone for cardiovascular and systemic health. Any disruption or inefficiency along its pathway can contribute to a kind of chronic imbalance, leading to stress, inflammation, and a host of common ailments that lower quality of life. For anyone facing heart or mood challenges, tuning into vagus nerve function is no longer optional; it’s foundational.
Role of Vagus Nerve in Homeostasis and Mental Health
Homeostasis—the body’s ability to maintain inner stability—is impossible without an optimally functioning vagus nerve. It modulates heart rate, blood pressure, digestion, and even immune responses, restoring calm after stress or exertion. Activating vagus nerve means empowering this process, which is especially vital in our chronically stressful environments.
There’s also a profound mental health connection: The vagus nerve guides the “rest and recover” branch of the nervous system. As studies in the International Journal of Neuropsychopharmacology detail, sustained nerve stimulation can alleviate anxiety and improve mood—even in cases of resistant depression. Attention to this system offers hope to those for whom standard therapies offer poor sustainability of benefit. The mind-body relationship isn’t just a metaphor; it’s a mechanism rooted in the vagus nerve itself.

The Link Between Vagus Nerve and Resistant Depression
For those suffering from treatment resistant depression, the vagus nerve carries unique importance. When standard medications and therapy systems fall short, doctors are increasingly turning to vagus nerve stimulation as an adjunctive option. This isn’t science fiction—a wealth of clinical trials, including work at Washington University School of Medicine, shows that carefully targeted electrical pulses to the vagus nerve can spark a meaningful response in depressive symptoms.
But why does this work, when traditional therapies so often fail? It’s about circuit correction. The vagus nerve’s deep reach into brain centers associated with mood and motivation means that stimulating it can unlock new neural pathways and facilitate emotional regulation—sometimes for the first time in years. While not a universal cure, for the tens of millions struggling with depression have very poor response to treatment, this development signals powerful promise and real hope.
Activating Vagus Nerve: Current Theories and Debates
Nerve Stimulation: A Closer Look at Mechanisms
At its core, nerve stimulation involves triggering gentle electrical activity in the vagus nerve—either via implanted devices, transcutaneous (through the skin) methods, or behavioral techniques like deep breathing. Researchers are still debating exactly which approach delivers the most consistent results. Implantable vagus nerve stimulation, studied in a clinical trial, seems to have strong effects in severe cases of resistant depression and cardiac dysfunction. However, emerging studies suggest that simple, at-home practices also initiate changes in heart rate and inflammation markers.
The science is evolving, but key findings suggest that such stimulation produces a calming signal—reducing the “fight or flight” response, harmonizing electrical rhythms of the heart, and interrupting feedback loops driving chronic stress and disease. As with most biomedicine, there are nuances: effectiveness varies by person, and results are highly context-specific. Still, compared to traditional therapies, these techniques carry low risk and high upside.
Expert Opinions on Vagus Nerve Stimulation
Medical experts are increasingly vocal about the role of vagus nerve stimulation, particularly as evidence accumulates. According to Dr. Ann Walker, neuroscientist, “The vagus nerve is a critical player in tuning inflammation and heart rate. ” Her statement echoes a shift in mainstream thinking: stimulating this nerve impacts not just symptoms, but root physiologic processes across the body.
To be clear, there remain debates about optimal methods and long-term effects—especially when invasive electrical devices are used. Yet, the field is united on one point: ignoring the vagus nerve in cardiovascular and mental health strategies is a massive oversight. These expert opinions reflect a growing consensus that activating the vagus nerve should play a central role in both therapy and prevention.
“The vagus nerve is a critical player in tuning inflammation and heart rate,” says Dr. Ann Walker, neuroscientist.
Vagus Nerve Stimulation in Clinical Trial Research
Key Findings: Vagus Nerve Stimulation for Cardiovascular Health
Clinical trial research is rapidly reshaping our understanding of heart health. Studies published in journals like the International Journal of Neuropsychopharmacology underscore how vagus nerve stimulation directly influences heart rate variability, inflammation, and overall quality of life. Researchers found that subjects receiving vagus nerve intervention reported more stable blood pressure, reduced stress-induced heart events, and even better sleep—a powerful trifecta for cardiovascular resilience.
One standout clinical trial, conducted at the Washington University School of Medicine, demonstrated that vagus nerve stimulation generated clear benefits in patients with both heart conditions and depressive symptoms. These results are highly atypical—few interventions produce such cross-system improvements with minimal side effects. The key takeaway: this nerve represents a powerful, underutilized lever in heart and mental health care.
Clinical Trial Outcomes and Limitations
While the results are encouraging, it’s important to acknowledge the limitations. Not all individuals experience the same magnitude or duration of benefit—a concern highlighted by findings on poor sustainability of benefit in some patients. Certain trials also point to the necessity of individualizing therapy, given variability in nerve responsiveness and underlying health conditions.
The gold standard trials emphasize the need for further research, especially around the comparative effectiveness of traditional therapies and vagus nerve stimulation. Nevertheless, the low-risk nature of most nerve stimulation techniques—unlike many drug-based regimes—makes this approach a compelling adjunct to standard care for both heart and mood disorders.
| Therapy | Target Condition | Key Benefit | Limitations |
|---|---|---|---|
| Standard Heart Therapy System | Cardiovascular Disease | Improved outcomes in acute intervention | Poor sustainability of benefit, side effects |
| Vagus Nerve Stimulation | Cardiovascular Disease & Resistant Depression | Lower heart rate, better variability, improved mood | Inconsistent results, more research needed |
| Combined (Therapy + VNS) | Chronic Disease | Holistic improvement, lower relapse | Less studied, individualized outcomes |

Practical Ways of Activating Vagus Nerve
- Gentle cold exposure (such as brief ice baths or cool showers)
- Slow, deep breathing exercises
- Mindful meditation and prayer
- Chanting, humming, or singing
- Yoga and gentle exercise
- Social connectedness and laughter
Submerging the Body in an Ice Tub: Benefits and Cautions
One of the most talked-about techniques for activating vagus nerve is ice bath immersion. Brief cold exposure stimulates “the dive reflex,” automatically shifting the body into parasympathetic, vagus-dominated mode. The benefits are impressive: lower heart rate, improved blood flow, and a calming reset after emotional or physical stress. This method has gained popularity among athletes but is now entering mainstream wellness conversations as an accessible, non-pharmaceutical intervention.
However, caution is essential. Those with heart conditions, uncontrolled high blood pressure, or other medical issues should consult a professional before entering an ice bath. Even healthy individuals should start with shorter exposures and pay attention to their body’s signals. When used wisely, cold therapy complements other gentle nerve stimulation methods—amplifying results without strain.

Daily Habits for Activating Vagus Nerve
While occasional cold exposure can be transformative, daily habits are the true backbone of lasting vagus nerve resilience. Simple practices—such as slow, diaphragmatic breathing, mindfulness meditation, gentle movement (yoga, tai chi), and even humming or chanting—provide consistent stimulation that accumulates benefits over time. The daily function of the vagus nerve thrives on regular, subtle activation, not just peak experiences.
Even laughter and positive social interaction activate the vagus nerve. A routine centered on these habits fosters better heart health, stable mood, and enhanced quality of life. Remember: profound transformation often starts with the smallest, most consistent choices.
Resistant Depression and the Promise of Vagus Nerve Stimulation
Why Traditional Therapies Fail and How Nerve Stimulation Helps
For countless individuals, resistant depression is a complicated illness that makes everyday life a struggle, as standard treatments yield little or no response to treatment. Medications and therapy systems, while helpful for some, leave a significant percentage with lingering symptoms at the end of standard protocols—resulting in poor sustainability of benefit.
Nerve stimulation, particularly targeted to the vagus nerve, offers fresh hope. By introducing electrical pulses to key neural circuits, either through implantable devices or non-invasive techniques, biofeedback and mood can change. For many, this approach marks the first meaningful response after years of struggle with kind of chronic depression.
Vagus Nerve Research in Treating Resistant Depression
The scientific evidence is mounting. In a pivotal clinical trial led by Dr. Charles Conway and colleagues at Washington University School of Medicine, researchers found that vagus nerve stimulation produced greater reduction in depressive symptoms than any control. Notably, those given nerve stimulation therapy reported sustained benefit and improved quality of life, even after years of failed treatments.
While results are highly atypical in traditional therapy for this population, vagus nerve stimulation has been cleared for use in treatment-resistant depression by international regulatory agencies and US Centers for Medicare services. For individuals facing multiple relapses and diminishing options, this form of therapy may represent a breakthrough—and a reason to reconsider the neurobiology behind our moods.
The Broader Picture: Vagus Nerve Stimulation for Mental and Physical Health
- Decreased heart rate and improved variability for cardiovascular resilience
- Reduction in depressive symptoms and enhanced mood
- Greater stress tolerance and adaptive nervous system function
- Lower inflammation and immune system support
- Better sleep and improved daily function

Heart Rate, Stress, and the Parasympathetic Connection
The parasympathetic nervous system—driven by the vagus nerve—is designed to counterbalance stress, lowering heart rate, blood pressure, and cortisol. The more we practice activating the vagus nerve, the easier it becomes to slip into this restorative physiological state, even during life’s pressures.
This is not just a “nice to have” benefit. Chronic failure to shift gears from stress to calm underlies many cases of cardiovascular disease, mood disorders, and autoimmune flare-ups. With so many affordable, low-risk methods available, there’s little reason not to make vagus nerve health a daily priority for both mind and body.
People Also Ask About Activating Vagus Nerve
What is the fastest way to activate your vagus nerve?
Answer
The fastest way to activate your vagus nerve is through slow, deep diaphragmatic breathing. Studies show that exhaling longer than you inhale immediately signals the body to shift into a vagal, parasympathetic state. If you want to try a physical approach, brief exposure to cold (such as splashing your face with cold water or taking a short ice bath) can also prompt rapid nerve stimulation. For best results, combine both methods as part of a daily routine.
How does activating vagus nerve benefit the heart?
Answer
Activating the vagus nerve benefits the heart by reducing heart rate, stabilizing cardiac rhythms, and lowering inflammation—each critical for long-term heart health. This stimulation enhances heart rate variability, a marker of cardiovascular resilience, and helps buffer the effects of everyday stress. Over time, these adaptations can lower the risk of heart disease and support more efficient blood flow throughout the body.
Can vagus nerve stimulation help with resistant depression?
Answer
Yes, research—including major clinical trial studies—shows that targeted vagus nerve stimulation can significantly reduce symptoms in people with resistant depression. By delivering precise electrical pulses, this therapy can create measurable changes in brain circuits involved in mood regulation, often achieving positive results where medications and psychotherapy alone have failed.
FAQs on Activating Vagus Nerve
- Is vagus nerve stimulation safe? Most non-invasive methods are very safe; consult your doctor before using electrical devices or trying ice baths if you have heart problems.
- How often should I activate my vagus nerve? Daily practices such as mindful breathing or meditation are encouraged for sustainable benefit.
- Can children or older adults benefit from nerve stimulation? Yes—gentle methods like breathing, singing, and laughter are safe for nearly all ages and may improve daily function.
- How quickly will I notice effects? Some people feel immediate relaxation or a lower heart rate; deeper benefits accrue over weeks of consistent practice.
Key Takeaways on Activating Vagus Nerve for Wellness
- Vagus nerve stimulation is scientifically backed for heart, mood, and inflammation benefits.
- Gentle nerve stimulation methods like breathing, cold exposure, and mindfulness can be practiced daily.
- Clinical trial results show promise for overcoming resistant depression and improving quality of life.
- Integrating these practices can make a transformative impact on heart and whole-body health.
Personal Reflections: My Opinion on Integrating Vagus Nerve Practices
What I’ve Learned About Activating Vagus Nerve for Cardiovascular Health
After years of exploring wellness techniques—both as a writer and as a participant in my own health journey—it’s clear to me that activating the vagus nerve is among the most overlooked yet accessible ways to boost cardiovascular health. It takes little equipment, no prescription, and can fit seamlessly into daily routines. Whether through mindful breathing, an occasional ice bath, or simple meditation, these practices have changed my sense of resilience and calm, even during high-stress periods or when traditional methods disappointed.
In my view, no wellness strategy is complete without attention to the nervous system’s most powerful modulator. Science provides the blueprint, but daily experience forges the habit.
“Integrating vagus nerve stimulation into daily life can be transformative—but only when we balance science with experience.”

Next Steps: How to Begin Your Journey of Activating Vagus Nerve
Practical Tips to Get Started on Vagus Nerve Wellness
Start with what feels most natural. Choose a nerve stimulation technique—a minute of slow breathing, a gentle cold shower, or a short guided meditation—and practice daily for a week. Notice changes in heart rate, mood, or sleep. Track your experiences in a journal. Gradually layer in other methods, or lengthen your sessions as you feel comfortable. Remember, consistency outweighs intensity; it’s about building a new foundation for health, not heroics.
When to Seek Professional Guidance
If you have known heart issues, low blood pressure, or a history of major depression, consult your medical provider before beginning aggressive nerve stimulation methods like prolonged ice baths or high-tech devices. Doctors familiar with behavioral medicine or functional neurology can offer tailored advice and ensure that your nerve wellness journey complements existing therapies and maximizes results.
Explore More Wellness Insights
Visit https://thepassport2wellness.com/ for Evidence-Backed Health Resources
Conclusion: Activating your vagus nerve isn’t just a wellness trend—it’s a science-backed strategy for a longer, healthier life. Start today and notice the difference.
 Add Row
Add Row  Add
Add 



Write A Comment