Did you know? Nearly two-thirds of people in minor car accidents experience whiplash and neck pain within just 48 hours. Whether it’s the aftermath of a sudden fender-bender, a tumble in your favorite sport, or an unexpected slip at work, whiplash is more common—and more impactful—than most realize. This guide will walk you through the realities, symptoms, and best treatment options for whiplash injury, giving you the tools to take control of your recovery.
Staggering Reality: Whiplash and Neck Pain Statistics and Impact
Each year, millions of people worldwide endure whiplash injuries, making it one of the most common injuries sustained in both traffic accidents and recreational sports. Recent statistics highlight that over 2 million cases of whiplash occur annually in North America alone, with car accidents accounting for about 85% of these incidents. However, whiplash doesn't just stem from high-speed crashes—slow collisions, slips, and physical altercations also contribute significantly to its prevalence.
The personal and societal impacts are staggering. Chronic neck pain develops in up to 40% of those who experience a whiplash injury, leading to long-term discomfort, interruptions in daily activities, missed work, and considerable healthcare costs. The effects reach beyond the initial trauma, as untreated or poorly managed whiplash can result in lasting neck sprain, headaches, and reduced quality of life. Understanding these realities is the first step to prevention, prompt care, and lasting recovery.

Understanding the Widespread Effects of Whiplash Injury
Whiplash is not just a minor neck sprain—it’s a complex soft tissue injury that ripples through every aspect of an individual’s life. The physical symptoms are only the beginning; many sufferers grapple with emotional distress, difficulty concentrating, and severe limitations in work or recreation. In some cases, these effects persist for months, highlighting the need for a thorough evaluation by a care provider or healthcare provider.
Emotional and psychological impacts shouldn’t be underestimated. Fear of movement and anxiety about exacerbating the injury often deter patients from engaging in recommended exercises or daily activities, which unfortunately can slow recovery. The widespread prevalence of whiplash injuries and their multi-layered effects underscore why it’s vital for anyone with neck pain after an injury to pursue a professional evaluation and an individualized treatment plan.
"Did you know nearly two-thirds of individuals involved in minor car accidents experience whiplash and neck pain within 48 hours?"
What You’ll Learn About Whiplash and Neck Pain
Prevalence and causes of whiplash and neck pain
Key symptoms and warning signs of a whiplash injury
How to work with a healthcare provider or care provider
Step-by-step approaches to treat whiplash and recover faster
Proven at-home and professional treatment plans
When to seek immediate medical attention
Frequently asked questions and expert advice
What is Whiplash and Neck Pain?
Defining Whiplash Injury and Related Neck Pain
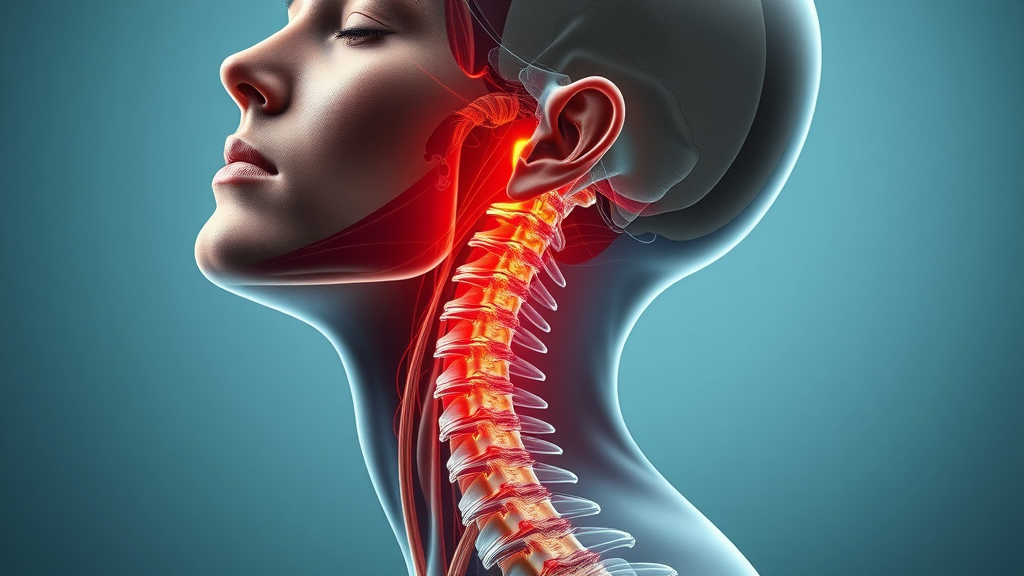
Whiplash is an injury of the soft tissues—muscles, ligaments, and tendons—in the neck that typically results from a rapid back-and-forth or side-to-side movement of the head and neck. This sudden movement, often described as the motion of a cracking whip, places extreme stress on the cervical spine and surrounding soft tissues. While the most common injury mechanism is a rear-end car accident, whiplash can also arise from sports collisions, falls, or other physical trauma.
Neck pain is the classic symptom, but whiplash is a neck injury that can manifest as muscle stiffness, headaches, restricted range of motion, or tingling in the arms and shoulders. Because the soft tissues are involved and damage is not always visible on basic X-rays, a physical exam and detailed patient history are often key in diagnosing whiplash. Prompt recognition and intervention can help prevent the development of chronic pain and long-term disability.
Mechanism: How Whiplash Injuries Occur
A typical whiplash injury occurs when the head and neck are suddenly thrown backward and then forward (or side-to-side), causing the cervical spine to extend beyond its normal range. This sudden movement—whether from a low-speed car accident or a hard tackle in sports—can stretch or tear the neck’s soft tissues and even result in minor damage to the intervertebral discs or joints.
While high-speed impacts increase the risk, it is a misconception that only serious crashes cause whiplash. In reality, even slow collisions at speeds as low as 5 mph can produce sufficient force to injure the muscles and ligaments of the neck. Both the magnitude and the direction of the force play a role in determining the severity of the injury, making it important to take any neck pain following an accident seriously.
"\"A whiplash injury isn’t only for high-speed crashes; it can happen even at speeds as low as 5 mph,\" notes a leading healthcare provider."
Common Causes of Whiplash and Neck Pain
Automobile accidents
Sports injuries
Slips and falls
Physical assault
Repetitive work or poor ergonomics
Rear-end car accidents remain the leading cause of whiplash and neck pain, but other activities—such as diving, contact sports like football, or even a forceful shake—can lead to the same injury. Poor posture, improper workstation setup, or repetitive movements in certain jobs can also create chronic strain, increasing the likelihood of a neck injury.
Not all neck pain arises suddenly; some cases develop gradually through microtrauma and overuse, especially if daily activities frequently involve awkward head and neck positions. By understanding the diverse causes, individuals and providers can more accurately assess risk and pursue the correct interventions to treat whiplash.
Recognizing Symptoms of Whiplash and Neck Pain

Primary Whiplash Symptoms: What to Look Out For
The common symptoms of whiplash often develop within hours or days following an injury. Typical signs include aching, stiffness, and pain in the neck, headaches at the base of the skull, pain radiating into the shoulders or upper back, and reduced range of motion. Some individuals may notice discomfort with movement, muscle spasms, or sensitivity to touch over the affected area.
Additional symptoms of whiplash include dizziness, blurred vision, and fatigue. Tingling or numbness in the arms may indicate involvement of nerve structures, which requires urgent assessment by a healthcare provider. Many of these issues intersect with those from other neck injuries, so a precise diagnosis by a care provider is important for designing the right treatment plan.
Delayed Symptoms of Whiplash Injury
Some symptoms of whiplash may not emerge until days or even weeks after the incident. These delayed effects can include persistent headaches, difficulty sleeping, problems concentrating, memory disturbances, or chronic neck pain. Emotional symptoms such as irritability, depression, or anxiety are also possible, particularly if pain disrupts normal function or quality of life.
Because delayed symptoms can complicate recovery, it’s crucial to monitor for signs beyond immediate pain. If discomfort increases or new symptoms develop, revisit your healthcare provider to reassess your treatment plan. Comprehensive care, including follow-up visits, ensures the underlying injury is treated—reducing the risk of developing chronic pain.
Immediate Symptoms |
Delayed Symptoms |
|---|---|
Pain and stiffness in neck |
Chronic neck pain or headaches |
Reduced neck mobility |
Difficulty sleeping |
Headaches at the skull base |
Problems concentrating |
Dizziness |
Memory issues |
Shoulder/upper back soreness |
Fatigue, mood changes |
How Long Does Whiplash Neck Pain Last?
The duration of whiplash and neck pain varies widely, depending on the injury's severity, promptness of care, and individual factors like age and overall health. For most, pain and stiffness improve within one to three weeks. Mild cases often resolve with conservative measures such as rest, gentle stretching, and guidance from a care provider.
However, up to 40% may experience symptoms beyond three months—a condition sometimes called “late whiplash syndrome.” Factors like severe initial pain, neurological symptoms, or lack of timely treatment increase the risk of developing chronic pain. Early intervention by a healthcare provider and a tailored treatment plan dramatically boost the chance of a full recovery.
When to Seek Medical Help: Role of Your Care Provider and Healthcare Provider
Red flag symptoms: severe pain, neurological changes
Unrelenting headache or weakness
Loss of bladder/bowel control
It’s critical to contact a healthcare provider promptly if you develop severe neck pain, persistent headaches, numbness or tingling in your arms, loss of balance, or new issues with bowel or bladder control. These "red flag" symptoms may signal more serious injuries, such as cervical spine fractures or nerve involvement, requiring emergency intervention.
A qualified care provider will perform a physical exam, review your medical history, and possibly order imaging studies—such as X-rays or CT scans—if red flags are present to rule out serious conditions. Prompt diagnosis and coordinated care can help avoid complications and optimize your recovery, especially if you experience prolonged or worsening symptoms.
How Do Doctors Determine Whiplash?

Diagnosing a whiplash injury involves a combination of patient history, a focused physical exam, and, in some cases, imaging studies. Doctors will ask about the incident, assess your neck movement, test for signs of nerve irritation, and palpate the soft tissues for tenderness and muscle spasm. They will also look for neurological signs—such as weakness or sensory loss—that would warrant further evaluation.
CT scans and X-rays are generally reserved for cases with red flag symptoms or when serious bone injury is suspected. Most whiplash cases involve injury to soft tissues that do not appear on standard imaging, making the expertise of your healthcare provider essential for designing a personalized treatment plan. Communication with your care provider about all symptoms, including those that arise later, is key for safe and optimal recovery.
How to Relieve Whiplash: Evidence-Based Approaches
Acute Care Plan: Immediate Steps After Whiplash Injury
Early management is crucial in relieving whiplash and neck pain. Immediately after injury, applying ice to the affected area for 15–20 minutes every 2–3 hours can help limit swelling and ease discomfort. Gentle movement within pain-free limits is usually encouraged—total immobility may delay healing unless specifically advised by your care provider. Over-the-counter options like acetaminophen or nonsteroidal anti-inflammatories (NSAIDs) can be used for acute pain.
For some, a soft cervical collar may be prescribed briefly—typically for no more than 48 to 72 hours—as prolonged immobilization can weaken neck muscles and prolong symptoms. Consulting with a healthcare provider will allow for rapid assessment and adjustments to the immediate care plan as needed, reducing the risk of long-term problems.
Physical Therapy and Rehabilitation: The Cornerstone of Whiplash and Neck Pain Recovery

Physical therapy is the cornerstone of most recovery plans for whiplash injuries. A skilled therapist will design exercises to gently restore neck range of motion, improve strength, and decrease muscle tension. This hands-on approach prevents stiffness, reduces the risk of chronic pain, and builds confidence in returning to normal activities.
Techniques may include manual therapy, targeted stretching, postural training, and modalities such as heat, cold, or electric stimulation. Each program is customized, often progressively increasing activity based on improvement. Consistent follow-ups with your care provider or healthcare provider ensure the treatment plan remains effective as your symptoms evolve.
Medications, Injections, and Other Medical Treatment Plans
In cases where pain is moderate to severe, doctors may recommend short-term use of prescription medications or consider muscle relaxants to ease severe spasm. For persistent pain, targeted injections—such as trigger point injections or nerve blocks—may be considered. These treatments are typically adjuncts, supporting more active rehabilitation like physical therapy.
Non-pharmacological options, including mindfulness, manual therapy, and acupuncture, have shown promise in some cases for reducing chronic symptoms. Discussing all available modalities with your healthcare provider ensures that your treatment plan is comprehensive, evidence-based, and responsive to your unique needs.
How Do You Treat Late Whiplash Syndrome?
Post-concussion symptoms or chronic neck pain lasting beyond three months may represent “late whiplash syndrome.” Management requires a multidisciplinary approach—typically involving a combination of physical therapy, pain management, behavioral strategies, and sometimes consultation with a specialist. Chronic pain should be addressed proactively to prevent further limitations in work, recreation, and relationships.
Persistence of symptoms despite standard care may warrant advanced interventions, such as multidisciplinary pain clinics, counseling for anxiety or depression, and specialized rehabilitation programs. Detailed reassessment by a knowledgeable care provider is vital to identify overlooked issues and optimize your treatment plan for the best possible recovery.
Do’s and Don’ts: How to Treat Whiplash at Home
Gentle movement and stretches (with illustrations)
Ice vs. heat therapy
Rest vs. activity guidance
Over-the-counter medication options
Warning signs to stop

To treat whiplash at home, initiate gentle stretches and low-impact exercises as advised by your care provider. Begin with ice for the first 48 hours to reduce swelling, then transition to heat packs for muscle relaxation. Avoid extended bed rest; instead, maintain regular daily activities as tolerable without aggravating your symptoms.
Over-the-counter pain medications can help manage discomfort, but always consult with your healthcare provider regarding safe dosages and combinations. Stop exercises immediately if you experience sharp pain, numbness, weakness, or severe headaches. Proper home care supports faster recovery, but timely follow-up with your provider remains crucial for safety and lasting results.
Expert Insights: Working With Your Healthcare Provider or Care Provider
"Timely collaboration with your healthcare provider creates the best personalized treatment plan for whiplash and neck pain recovery."
Securing expert medical guidance is essential for optimal recovery from whiplash and neck pain. Your healthcare provider will track your symptoms, monitor healing, and adjust interventions as necessary. Honest communication about your pain, functional limitations, and any new or worsening signs will help your provider choose effective, evidence-based treatments.
Your care provider may also connect you with other specialists—physical therapists, pain management experts, or psychologists—to address every aspect of your recovery. Building this partnership ensures your plan adapts to changes and maximizes your chance for a full, lasting return to wellness.
Watch a brief educational video with expert narration and clear animations to understand the mechanics, common symptoms, and best-practice recovery solutions for whiplash injuries.
Frequently Asked Questions on Whiplash and Neck Pain
What are the most common symptoms of whiplash?
The most frequent symptoms of whiplash injury include neck pain and stiffness, headaches, reduced neck motion, shoulder discomfort, muscle tenderness, and sometimes tingling or weakness in the arms. Less common symptoms may involve dizziness, blurred vision, and fatigue. If you experience any neurological signs such as numbness, weakness, or loss of bladder/bowel control, seek immediate medical care.When should I see a healthcare provider?
You should contact a healthcare provider if you have significant neck pain following trauma, experience worsening or persistent symptoms, develop numbness or tingling in your limbs, or have severe headaches that don't improve. Timely medical evaluation ensures serious injuries are ruled out and that you receive an appropriate treatment plan.Can you prevent whiplash during car accidents?
While it’s not always possible to completely prevent whiplash injuries, you can reduce your risk by ensuring your headrest is properly adjusted, wearing your seatbelt at all times, sitting upright, and practicing defensive driving habits. These steps are especially important during rear-end collisions.Are alternative therapies effective for whiplash and neck pain?
Complementary approaches—such as acupuncture, manual therapy, and yoga—may offer additional relief for some individuals. However, these should supplement, not replace, evidence-based interventions like physical therapy. Always consult your healthcare provider before trying new treatments.
Key Takeaways on Whiplash and Neck Pain
Recognize the wide range of injuries and symptoms
Prompt diagnosis and treatment is essential
Recovery may require multi-modal care and patience
Consult your healthcare provider for any persistent or worsening symptoms
Conclusion: Take Action for Whiplash and Neck Pain Recovery
Act quickly, partner with your care provider, and follow evidence-based treatments for the best chance at a full recovery from whiplash and neck pain.
CAll Us at 905-354-5153
If you or a loved one are struggling with whiplash and neck pain, don’t wait. Compassionate, expert help is a phone call away—reach out today for a personalized assessment and recovery plan tailored just for you.
 Add Row
Add Row  Add
Add 



Write A Comment