Why Navigating Reimbursement Can Feel Like an Uphill Battle
Have you ever received a medical bill that didn’t match what you expected—or worse, felt a growing sense of dread after a treatment because you weren’t sure what insurance would or wouldn’t cover? For many patients, tackling reimbursement issues can be the most confusing and stressful part of receiving healthcare, especially when already coping with injury or pain. In physical therapy, these challenges don’t just impact your wallet. They can disrupt your sense of security, delay much-needed treatments, and create tension at a time you should be focusing on recovery.
The value of understanding reimbursement structures and processes cannot be underestimated. Many people confront a maze of terms, paperwork, and phone calls, uncertain where to start or how to appeal if something goes wrong. Unfortunately, this lack of clarity often leads to delayed care, frustration, and even lost benefits. Demystifying reimbursement is not just about paperwork—it's about regaining peace of mind and ensuring that people receive the support and solutions they need swiftly and with as little hassle as possible.
As we break down the realities of reimbursement in the context of physical therapy, it becomes clear: this is a pressing issue for individuals and families alike. Whether you’re a new patient navigating your first treatment or someone returning to physical therapy after a previous experience, understanding how to prevent, address, and resolve reimbursement issues is essential. By delving deeper, you’ll gain tools and strategies to move from confusion to clarity—so you can return your attention to what truly matters: your health and recovery.

Understanding Reimbursement: What It Really Means for Your Health and Wellness
Reimbursement refers to the process by which patients or healthcare providers receive payment from insurers for medical services provided. When it comes to physical therapy, reimbursement can be especially complex because of unique insurance policies, varied coverage for different conditions, and changing guidelines. Terms like “in-network,” “deductibles,” and “out-of-pocket maximums” only scratch the surface, leaving many patients genuinely unsure about what costs they will be responsible for and what support their insurance will actually provide.
Reimbursement issues can leave patients feeling caught in the middle—between care they need and the uncertainty of what they’ll owe. Without a good grasp of the reimbursement process, individuals might postpone treatment, accept limited rehabilitative care, or get stuck paying more than necessary. Immediate action is needed when clarity is lacking. The result of inaction isn’t just a financial hit; it could mean longer recovery times, persistent pain, or even stoppage of therapy. Addressing reimbursement challenges is about more than money—it's a key factor in achieving optimal health outcomes and sustainable wellness.
How a Clear Reimbursement Process Translates to Real Results in Physical Therapy
Expert-driven physical therapy facilities understand that a seamless reimbursement process can make all the difference for their patients. By clearly outlining financial responsibilities, assisting with insurance queries, and ensuring transparent billing, these practices reduce unnecessary stress and make every session more productive. With knowledgeable staff dedicated to demystifying the process, patients focus on healing instead of worrying about paperwork or unexpected expenses. Putting patient education at the forefront helps demystify terms, requirements, and deadlines that often complicate reimbursement, empowering individuals to make informed decisions about their care.

The ripple effect of a straightforward, well-managed reimbursement process is profound. Individuals undergoing physical therapy for injury recovery or chronic pain management benefit from uninterrupted care, secure in the knowledge that their treatment will not break the bank or come with hidden surprises. Insurance assistance and skilled administrative support also mean claims are processed faster and appeals are made efficiently—reducing delays in payment and eliminating much of the anxiety that often accompanies prolonged billing disputes. Ultimately, a transparent and supportive approach to reimbursement leads to better health, improved outcomes, and a less stressful patient experience.
Why Clarity in Reimbursement Matters for Lasting Recovery
For many, the journey to recovery hinges not only on quality physical therapy but also on unobstructed access to that care. When the reimbursement process is clear and predictable, patients can commit to their prescribed sessions, follow home exercise plans, and achieve their rehabilitation goals. Those recovering from injuries or managing chronic conditions often require ongoing therapy. A muddied or inconsistent reimbursement experience can discourage perseverance or even force patients to stop before they reach their full potential.
Empowered Patients: Tips for Navigating the Reimbursement Maze
Armed with clear, actionable information, patients can take active steps to smooth their reimbursement journey from the start. Keeping thorough records, asking pointed questions before treatment begins, and understanding the details of their insurance plan puts the power back in the patient’s hands. With the right guidance, reviewing an explanation of benefits, tracking claims, and swiftly addressing discrepancies or denials becomes manageable—not overwhelming. This approach builds confidence and ensures that financial considerations never overshadow personal health and wellness.
Looking Ahead: Evolving Solutions for Hassle-Free Reimbursement
Reimbursement challenges are evolving, and so are the solutions. As physical therapy practices adopt newer technologies and streamlined processes, the potential for billing errors, misunderstandings, or long wait times diminishes. The future points to greater transparency, digital communication with insurance providers, and more robust patient education programs. Staying informed about industry advancements equips patients to recognize—and demand—smooth, efficient reimbursement processes wherever they seek care, helping to safeguard their time, resources, and well-being.
Active Physical Therapy’s Commitment to Transparent, Supportive Reimbursement Practices
At Active Physical Therapy in Salisbury, transparency and patient empowerment stand at the forefront of their approach. Rather than treating reimbursement as a back-office hassle, the team integrates financial clarity into the overall care experience. By making it easy for each patient to understand their responsibilities and insurance coverage, Active Physical Therapy helps reduce financial anxiety and reinforce trust throughout the rehabilitation process. Every individual receives personal attention, ensuring they feel supported not only during recovery but also throughout their financial journey.
The philosophy at Active Physical Therapy includes compassionate education and a willingness to walk patients through every step of the reimbursement cycle. Staff is equipped with the knowledge, warmth, and patience to tackle insurance questions, help fill out paperwork, and act as advocates when issues arise. This commitment extends far beyond business hours—it is part of a broader mission to treat the whole person, not just the injury. The result is a supportive environment where patients can focus on regaining strength and mobility while knowing their financial well-being is in capable hands.

How Real People Experience Stress-Free Care and Reimbursement Success
Every patient’s experience with reimbursement has the potential to shape their entire outlook on recovery. Those who receive not only quality care but also practical help with billing and insurance report relief, gratitude, and a renewed sense of hope. As one patient recently shared, their journey was marked not only by expert staff and personalized therapy but also by the genuine support they felt from their very first encounter.
I've had the pleasure of doing physical therapy at Active physical therapy and I would love to say the staff there where very much so an awesome group& they took very amazing care of me Vera the physical therapist, Candace the tech & Barbara at front desk. They make you feel like new again in spite of your injuries sustained. I would tell everyone get over to active physical therapy and let them take wonderful care of you it's Amazing 😍😍😍😍
This firsthand perspective shines a light on the power of pairing expert rehabilitation with attentive support throughout the reimbursement process. Success stories like these carry a message: with the right guidance, others can move past barriers and enjoy a smoother, more confident path to healing.
Redefining the Standard for Reimbursement in Physical Therapy
As healthcare environments become more complex, streamlined reimbursement practices are essential to creating a supportive, patient-centered experience. Insights from practices like those at Active Physical Therapy demonstrate that with clear guidance and dedicated assistance, reimbursement obstacles can be quickly resolved or avoided entirely. By focusing on transparency, education, and patient advocacy, physical therapy clinics set a new standard—one where the stress of reimbursement no longer overshadows the importance of healing and renewed mobility. Through this lens, reimbursement is not just a transaction, but a critical aspect of whole-person care, ensuring that the journey to recovery remains focused on progress, empowerment, and peace of mind.
Contact the Experts at Active Physical Therapy
If you’d like to learn more about how reimbursement could benefit your physical therapy care, contact the team at Active Physical Therapy.
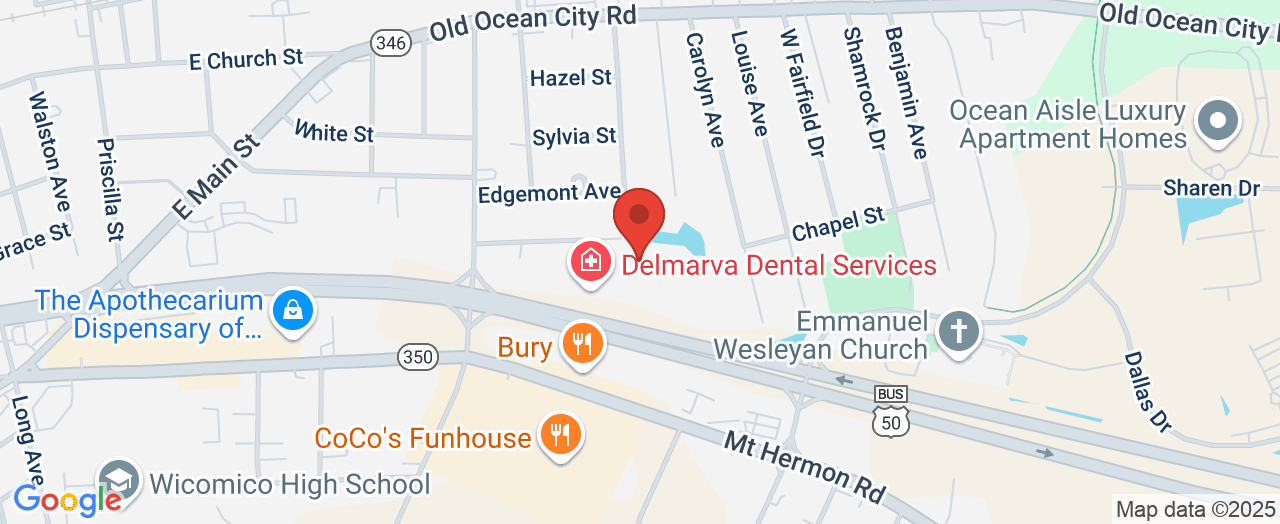
📍 Address: 1324 Belmont Ave STE 101, Salisbury, MD 21804, USA
📞 Phone: +1 410-656-9953
🌐 Website: https://www.active-physicaltherapy.com/Active-Physical-Therapy-in-Salisbury-MD.aspx
Active Physical Therapy Location and Availability
🕒 Hours of Operation:
📅 Monday: 8:00 AM – 7:00 PM
📅 Tuesday: 8:00 AM – 7:00 PM
📅 Wednesday: 8:00 AM – 7:00 PM
📅 Thursday: 8:00 AM – 7:00 PM
📅 Friday: 8:00 AM – 4:00 PM
📅 Saturday: ❌ Closed
📅 Sunday: ❌ Closed
 Add Row
Add Row  Add
Add 




Write A Comment